Paediatric Sleep Medicine Clinical Network
The Sleep Medicine Clinical Network was developed in 2014 and transitioned to the Respiratory and Sleep Clinical Network in September 2023.
The purpose of the New Zealand Paediatric Sleep Medicine Clinical Network was to support New Zealand health care professionals working across community, primary, secondary and tertiary services to deliver an equitable, high quality, cost effective and integrated sleep medicine service for children, young people and their families/whanau.
The New Zealand Paediatric Sleep Medicine Clinical Network provided clinical leadership in the development and maintenance of the nation-wide clinical service for children and young people up to 15 and when appropriate, 18 years of age, aiming to meet basic international benchmark standards.
If you would like to contact us for further information, please email respiratory@paediatrics.org.nz
Guidelines and articles
Sleep Disordered Breathing (SDB)
The New Zealand Guidelines for the Assessment of Sleep-Disordered Breathing in Childhood 2014 was produced by the National Paediatric Sleep Medicine Clinical Network as an evidence-based summary for the assessment of children with sleep disordered breathing. It aims to address the following clinical management issues for paediatric health care professionals in New Zealand:
How should general practitioners and paediatricians approach the investigation of a child who snores?
Which children should be referred from around New Zealand to a sleep disorders centre for further evaluation?
What treatments are available for disorders of breathing during sleep in childhood and what are the known benefits of these treatments?
Full guideline: a pdf copy of the full guideline: New Zealand Guidelines for the Assessment of Sleep Disordered Breathing in Childhood 2014 can be downloaded here: https://media.starship.org.nz/guideline-for-the-assessment-of-sleep-disordered-breathing-in-childhood/Final_PSNZ_SDB_guideline_2015_plus_Exc_sum.pdf
Summary: This link provides a summary of the New Zealand Guidelines for the Assessment of Sleep-Disordered Breathing in Childhood 2014. This guideline is intended for GPs and paediatricians involved in the care of children and young people 2 years and older: https://www.starship.org.nz/guidelines/sleep-and-sleep-disordered-breathing-in-children
NZ Regional Clinical Pathways
Access to regional clinical pathways are available through the Goodfellow Unit at this link: https://www.goodfellowunit.org/clinical-pathways and the Health Navigator website at this link: https://www.healthnavigator.org.nz/clinicians/r/regional-pathways/
These supply links to the clinical pathways within each main region of New Zealand. Pathways are localised for each region and access is limited to health providers. If you do not know the login details, you will need to contact your DHB or PHO for more information.
The Paediatric Sleep Medicine Clinical Network has been involved in the development of the Canterbury Community HealthPathways: Snoring and Sleep Apnoea in Children and Sleep Problems in Children. Further information for this pathway can be found below:
Canterbury Community HealthPathways: Snoring and Sleep Apnoea in Children and Sleep Problems in Children
HealthPathways offers clinicians locally agreed information to make decisions, together with patients, at the point of care. The Canterbury HealthPathways suite includes Community HealthPathways, which provide general practice teams with information to consistently assess and manage medical conditions, as well as the criteria for requesting health services in the Canterbury DHB. Written for general practice teams, Community HealthPathways is also useful to all other health professionals.
A link to a pathway on ‘Snoring and Sleep Apnoea in Children’ can be found under the ‘Child and Youth Health’ section; ‘Respiratory -Child’:
https://canterburydraft.communityhealthpathways.org/index.htm?441470.htm
https://canterburyclassicdraft.communityhealthpathways.org/index.htm?441470.htm?stayonsite=1
A link to the pathway on ‘Sleep Problems in Children’ can be found under the ‘Child and Your Health’ section; ‘Behaviour and Development – Child’: https://canterburydraft.communityhealthpathways.org/469263.htm
Obstructive Sleep Apnoea
Obstructive sleep apnoea syndrome (OSA) is a relatively common and potentially serious medical condition in children causing sleep disruption and abnormal physiology. A guideline in regard to OSA can be found here: https://www.starship.org.nz/guidelines/obstructive-sleep-apnoea/
Oximetry
A guideline intended to assist clinicians with the performance, reporting and interpretation of paediatric overnight pulse oximetry studies can be found here: https://www.starship.org.nz/guidelines/oximetry/
Sleep and Sleep Disordered Breathing in Cystic Fibrosis.
Chronic respiratory disease such as cystic fibrosis can be associated with sleep disturbance due to problems such as cough, wheeze, nasal obstruction or side effects of medication. A guideline in relation to this can be found here: https://www.starship.org.nz/guidelines/sleep-and-sleep-disordered-breathing-in-cystic-fibrosis
Melatonin
Melatonin is increasingly being used to facilitate sleep in the paediatric population. This article reviews the indications for melatonin in children, and the evidence of benefits and of safety for melatonin use by children presenting with difficulty falling asleep or maintaining sleep.
NZ Doctor 16 August 2019 Pg 38 - Melatonin as an aid to a child's sleep? A cautionary note.
Another relevant link regarding melatonin use: https://bpac.org.nz/BPJ/2015/August/melatonin.aspx
Tools and questionnaires
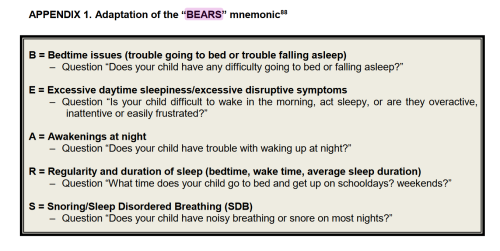
BEARS mnemonic
The BEARS mnemonic can be used as a guide for history taking. Parents should be asked about snoring or noisy breathing in particular.
https://www.starship.org.nz/guidelines/sleep-and-sleep-disordered-breathing-in-children/ (page 48)
Chamness JA. Taking a pediatric sleep history. Pediatr Ann 2008; 37:502-508.
Paediatric OSA screening questionnaire
If symptoms of snoring or noisy breathing are noted, a paediatric OSA screening questionnaire should be completed https://media.starship.org.nz/osas-screening-questionnaire/osas_screening_questionnaire.pdf This questionnaire is based on the Chervin Paediatric Sleep Questionnaire.
For the linked questionnaire add up the "Yes" scores for the 22 items. A score greater than 7 with no missing items, or a percentage value of 0.33, has a 78% sensitivity and a 72% specificity for detecting polysomnograph (PSG) diagnosed OSA (AHI >5).
Paediatric Sleep Questionnaire (PSQ)
Access to an electronic version of the PSQ will be available through the Whanau Pakari project - an electronic link to the PSQ will be uploaded when available.
Guidance for the assessment and management of children with sleep disordered breathing
For further guidance for the assessment and management of children with sleep disordered breathing see NZCYCN guideline on sleep disordered breathing, including a suggested pathway (Appendix 3). This is also outlined and summarised in the OSA guidelines on the Starship website: https://www.starship.org.nz/guidelines/obstructive-sleep-apnoea/
Pictures of Tonsil size
The size of the tonsils is graded on a scale from one to four. Four is the largest size. The tongue should be rested comfortably in the mouth for best judgment of the tonsil. Palatine tonsils are graded based on how much the airway is obstructed due to the tonsil protruding from either side of the oropharynx.
Brodsky grading scale: The Brodsky grading scale is comprised of the following 5 grades:
Grade 0: Tonsils are absent or have been removed. Tonsils are within the tonsillar fossa.
Grade 1: Tonsils are barely visible. This is the normal tonsil size. It indicates that the tonsil extends to the pillars. Tonsils are just outside of the tonsillar fossa and occupy ≤25% of the oropharyngeal width.
Grade 2: the tonsillar tissue is not beyond the tonsillar pillars. This is also normal tonsil size. Tonsils occupy 26-50% of the oropharyngeal width.
Grade 3: The tonsils are enlarged. Can be seen with infection. It indicates that tonsils extend beyond the pillars but stop short of the midline. Tonsils occupy 51-75% of oropharyngeal width.
Grade 4: Tonsils extend to the midline and are almost touching each other. Seen with significant infection. Tonsils occupy >75% of oropharyngeal width.
Video of child with OSA
Oximetry Learning Tool
This educational tool would be most useful for paediatric trainees and paediatricians, as well as other paediatric health professionals. The course is password protected. The instructions on how to access it are as follows:
To find the course go to: https://www.goodfellowunit.org/
If you are not a member of Goodfellow Unit you must first register (this takes 2 minutes)
Once signed in go to the website homepage. At the bottom of that page you will see 'Enter Package Code'
Enter the code Oxi06 and hit ‘Submit’
Information for clinicians and families
Kidshealth
The KidsHealth website has been created by a partnership between the Paediatric Society of New Zealand (PSNZ) and the Starship Foundation, supported and funded by the Ministry of Health. The aim of this website is to provide New Zealand parents, caregivers, family and whānau with accurate and reliable information about their children's health. Visit https://www.kidshealth.org.nz to see a range of information developed for parents and caregivers. These are the main links on the Kidshealth website about sleep and there are many relevant factsheets within each link:
This link https://www.kidshealth.org.nz/tags/sleeping-sound leads to information about:
- Normal sleep
- Sleep problems
- Tools for Managing Sleep Problems
This link https://www.kidshealth.org.nz/tags/sleep leads to information about:
- Problems getting to sleep
- Night Terrors
- Restless Legs syndrome
- Sleep and breathing problems in Neuromuscular conditions
- Bedtime resistance
- Nightmares
- Sleep and anxiety
- Positional head flattening in babies
- Delayed sleep
- Night waking problems
- Sleep Associations
- Polysomnography (Sleep Study)
- Insomnia
- Snoring or noisy breathing in children
- Overnight oximetry
Example of Rapid Eye Movement (REM) sleep in an infant (video)
Often parents can misinterpret an infant in REM sleep for being awake or waking up and can possibly disturb an infant’s sleep. Here is an example of REM sleep, which may be helpful to show families, so they can distinguish REM sleep: https://www.youtube.com/watch?v=AZ6I9N7t7Vc
Ministry of Health
The Ministry of Health https://www.health.govt.nz/ has also produced information and factsheets about sleep. These include:
Baby sleep and settling: https://www.health.govt.nz/your-health/pregnancy-and-kids/first-year/helpful-advice-during-first-year/baby-sleep-and-settling
Helping young children sleep better: https://www.health.govt.nz/your-health/healthy-living/food-activity-and-sleep/sleeping/helping-young-children-sleep-better
Helping children sleep better: https://www.health.govt.nz/your-health/healthy-living/food-activity-and-sleep/sleeping/helping-children-sleep-better
Helping teenagers to sleep better: https://www.health.govt.nz/your-health/healthy-living/food-activity-and-sleep/sleeping/helping-teenagers-sleep-better
Sleep problems: https://www.health.govt.nz/your-health/conditions-and-treatments/diseases-and-illnesses/sleep-problems
Health Navigator NZ
The Health Navigator website https://www.healthnavigator.org.nz provides a place for New Zealanders to find reliable and trustworthy health information and self-care resources. It is a non-profit community initiative combining the efforts of a wide range of partner and supporter organisations, and is overseen by the Health Navigator Charitable Trust. Some links with sleep related information for families from this website include:
Why sleep is important and stages of sleep: https://www.healthnavigator.org.nz/healthy-living/s/sleep-importance-of/?tab=15345#Overview
Sleep for babies: https://www.healthnavigator.org.nz/healthy-living/s/sleep-for-babies/
Sleep and children and sleep problems in children: https://www.healthnavigator.org.nz/healthy-living/s/sleep-and-children/
Raising Children
Raising Children Media Ltd https://www.raisingchildren.org.nz/ is a media company set up to support parents by providing them with quality video content on subjects they'll find helpful. This is supported by the New Zealand Government. For example:
Newborn sleeping: http://www.raisingchildren.org.nz/stories/newborn-sleeping/
Sleeping in the early months: https://www.raisingchildren.org.nz/infant/#infant-sleeping
Sleeping for crawlers: https://www.raisingchildren.org.nz/crawler/#crawler-sleeping
Sleep from 1-3years: https://www.raisingchildren.org.nz/twoyears/#twoyears-sleeping
Sleep/Wake Research Centre Moe Tika/Moe Pai
The Sleep/Wake Research Centre, Massey University have developed a series of COVID19 resources regarding sleep. Each information sheet is also available as a downloadable PDF. https://www.sleepwake.ac.nz/what-we-do/covid-19-resources/
These include (each information sheet is also available as a downloadable PDF):
Sleep for parents and babies: https://www.sleepwake.ac.nz/what-we-do/covid-19-resources/sleep-for-parents-and-babies/
Children’s sleep (tips for parents): https://www.sleepwake.ac.nz/what-we-do/covid-19-resources/childrens-sleep-for-parents/
Children’s sleep (tips for children): https://www.sleepwake.ac.nz/what-we-do/covid-19-resources/childrens-sleep-for-children/
Sleep for teenagers: https://www.sleepwake.ac.nz/what-we-do/covid-19-resources/sleep-for-teenagers/
For further information on PSNZ / MoH Clinical Network development, please contact Clinical Networks Support Manager, Karyn Sanson, karyn.sanson@paediatrics.org.nz. |
