Parenchymal lung disease
Please note: images that have a white symbol at the top right, such as the RDS image below, indicates an image gallery that has multiple images - click on the image to open the gallery.
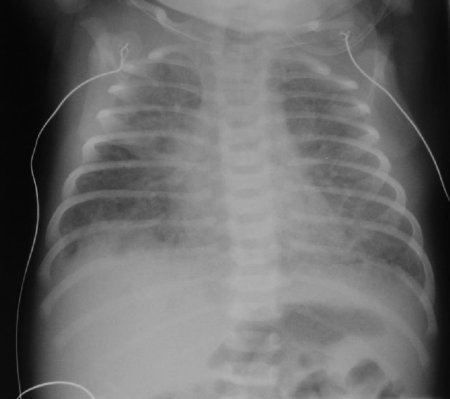
Respiratory Distress Syndrome (RDS)
Respiratory Distress Syndrome (RDS) is a clinical diagnosis but one which is often interchanged with the terms Hyaline Membrane Disease (a pathological diagnosis) and Surfactant Deficiency (a term describing the typical appearances on radiographs of infants with RDS).
The typical radiological features of Surfactant Deficiency are:
Small volume lungs
Homogenous "ground glass" opacity
Air bronchograms
These classical radiological appearances have been altered by interventions such as CPAP (which tends to result in lungs which are of normal size) and surfactant administration (which is often given prior to the radiograph being taken, and can result in less homogenous appearances).
The differential diagnosis includes:
Pneumonia (particularly Group B Streptococcus)
Retained Fetal Lung Fluid/TTN
Transient Tachypnoea of the Newborn (TTN)
Transient Tachypnoea of the Newborn (TTN, also called Retained Fetal Lung Fluid or "Wet Lung") is a diagnosis of exclusion.
Typical radiologic features are ill-defined but include:
Increased central vascular markings ("star-burst" appearance)
Hyperaeration
Evidence of interstitial and pleural fluid
Prominent interlobar fissures
Cardiomegaly
Because the symptoms and radiological features are non-specific, infection should be considered in the differential diagnosis. Typically, respiratory symptoms resolve within the first 24-hours of life, but occasionally can persist longer.
Pneumonia
The chest radiograph appearances of pneumonia are not specific, and frank lobar consolidation as seen in adults and older children is rare. More commonly, there is coarse opacity of one or more regions of the lung parenchyma.
However, these appearances can also be seen with retained fetal lung fluid, meconium aspiration, aspiration of gastric contents, and pulmonary haemorrhage.
Pleural effusions are not uncommon in infection, but again may be seen with other conditions.
Group B Streptococcus can have an appearance similar to Respiratory Distress Syndrome (Surfactant Deficiency), although the granulation is typically more coarse.
Meconium Aspiration Syndrome
Meconium stained amniotic fluid (MSAF) occurs in about 12% of deliveries.
Meconium aspiration is defined by meconium aspirated from below the vocal cords. However, Meconium Aspiration Syndrome (MAS) defines a wide array of respiratory symptoms associated with MSAF.
MAS usually presents as respiratory distress and cyanosis. Pulmonary hypertension is common.
The radiograph usually shows :
Coarse infiltrates
Widespread consolidation
Hyperinflation
Pleural effusions are not uncommon
Pneumothorax and pneumomediastinum may be present
Because the symptoms and radiological features are non specific, infection should be included on the differential diagnosis.
The images are from a term infant born through thickly stained meconium liquor.
The infant had initial respiratory distress. She developed cyanosis and an oxygen requirement. The initial two films show bilateral patch opacity with hyperinflation (although not severe).
She deteriorated and was ventilated. On the third image, she appears to have some air leak with a prominent mediastinal lucency and some free air at the bases. There is still patchy opacity of the lung fields.
She slowly improved after about a week of intensive care including inhaled nitric oxide, before being extubated. The final film shows the post-extubation film with right upper lobe collapse. She developed significant residual neonatal chronic lung disease and was discharged on low-flow oxygen at the age of one month.
Pulmonary Haemorrhage

Pulmonary haemorrhage is relatively common in neonates. It can be dramatic in its onset, with a catastrophic collapse, or it can be more subtle with blood-tinged endotracheal secretions. In preterm infants, it is most commonly associated with a patent ductus arteriosus causing haemorrhagic pulmonary oedema. Other causes include surfactant administration (perhaps from a rapid change in compliance resulting in an increase in the size of the left-to-right shunt, and haemorrhagic oedema), airway haemangiomata (rare), and any cause of pulmonary congestion (for example, severely reduced left ventricular function in an asphyxiated or septic term infant).
Chest radiographs are non-specific in appearance and commonly demonstrate patchy infiltrates, although appearances can be normal.
Babies frequently require a significant increase in their ventilatory support. The PEEP should generally be increased in an attempt to maintain high mean airway pressures so that oedema is forced back into the pulmonary vascular bed.
Neonatal Chronic Lung Disease
This is usually a sequel of significant lung disease in the immediate newborn period.
Classically, four stages were described by Northway in 1967.
Stage 1 was the homogenous appearance of RDS
Stage 2 was a generalised opacity, frequently seen towards the end of the first week of life
Stage 3 marked the onset of chronic changes, with a bubbly appearance
Stage 4 consisted of a inhomogenous appearance with hyperinflation, bleb formation, irregular fibrous streaks, and cardiomegaly (from cor pulmonale).
Other scoring systems have followed. These have largely been used in research rather than in clinical practice.
The first two radiographs show appearances at 8 and 12 days in a baby born at 25 weeks. The lung fields show a coarse bubbly appearance, initially more marked on the right but then more widespread a few days later.
The last radiograph shows advanced Stage 4 CLD. The infant is the same as in the PDA image on the "Cardiac Disease" radiology library. There is unevenness of the ribs on the left side following a PDA ligation. The lung fields are generally "bubbly" and "streaky" with localised areas of hyperaeration in the right lower lobe and left lower lobe.
The strongest risk factor for neonatal CLD is now gestation. Ventilation and oxygen may play a role in the pathogenesis, as may infection with organisms such as Ureaplasma.
Water Aspiration
Water birth is an uncommon practice in our institution and in those maternity hospitals who refer to our NICU. There is little evidence that water immersion has benefits to the mother, and even less evidence suggesting benefit to the infant. We have reported 4 cases of infants with neonatal illness who were born through water (Nguyen S, Teele R, Kuschel C, Spooner C. Waterbirth – a near drowning experience. Pediatrics 2002; 110 411-3).
Infants can be severely ill initially and require ventilation, but frequently they improve with mild respiratory support (oxygen and nasal CPAP). The chest radiographs are not specific but frequently demonstrate pleural effusions and patchy alveolar infiltrate.
Infection must be considered in the differential diagnosis, and antibiotics should be given at least until cultures are proven negative. There are reports in the literature of infants developing conjunctivitis with Pseudomonas and other water-borne organisms.
Hydrops
Hydrops describes a scenario of fluid in at least two body cavities. The images to the left demonstrate an infant with hydrops - in this case, bilateral pleural effusions, ascites, and oedema.
The first image demonstrates the appearance after birth. There is generalised oedema, bilateral huge pleural effusions, and the right lung is seen as the (small) lucent area slightly crossing the midline. Note the appearance of central gas in the abdomen, suggesting the presence of ascites.
Following the insertion of bilateral chest drains, there is residual fluid on the right side particularly. The endotracheal tube is low.
The third image demonstrates the appearance 3 days after birth. There has been a dramatic reduction in the subcutaneous oedema. Bilateral pleural effusions remain.
The cause of this baby's hydrops was thought to be a congenital chylothorax. He was managed with dietary manipulation using Monogen, without re-accumulation of his pleural effusions. He was changed to breast feeding uneventfully at three weeks of age.
The causes of hydrops are extensive, and management in the delivery room is critical with many babies requiring urgent insertion of chest drains, as well as abdominal paracentesis, in order to achieve effective resuscitation. Senior neonatal staff should be informed of the delivery and will usually attend.
Refer to the hydrops guideline for more information.
