6. Insulin types and regimens
Insulin Types/Action
| Ultra-Fast/Short Acting Insulin |
|
| Long Acting Insulin Analogues |
|
| Other Insulins |
| While less commonly used in children and young people, there are other types of insulin available in New Zealand. Your diabetes team will guide you if these are ever needed. These include:
|
Want to know more about insulin injections? Find out more...
Insulin regimens
Most children newly diagnosed in hospital start on injections using pens using a basal bolus regimen.
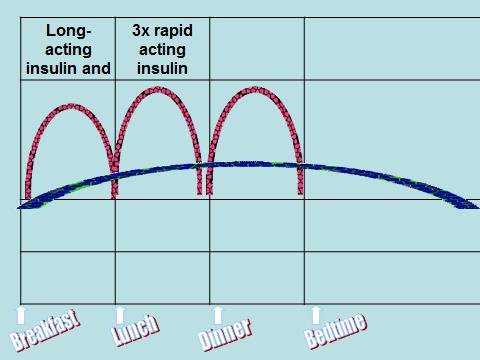
Basal bolus or MDI injections
A basal bolus insulin regimen is a way of managing diabetes that closely mimics how the body's natural insulin release. It involves using two types of insulin:
Basal insulin - This is long-acting insulin given once or twice a day to manage blood glucose levels between meals and overnight. It is often called "background insulin" because it supports the body's basic functions.
Bolus insulin - This is rapid-acting insulin given before meals to manage the rise in blood glucose after eating. It is sometimes referred to as "food insulin". Families will be supported to learn how to count carbohydrates so they can match the amount of bolus insulin to the food their child eats. This is known as the "carb ratio".
Correction factor - Also known as the "insulin sensitivity factor or ISF" , this is used to calculate additional insulin needed to lower high blood glucose levels. The correction dose is added to the food insulin if glucose levels are above target.
For example:
Food insulin + correction insulin = total dose
This approach offers more flexibility around mealtimes and helps achieve better blood glucose control.
You can read a transcript of this video here.
Insulin pumps
How do insulin pumps work?
An insulin pump is a small, battery-powered device that helps manage diabetes by giving insulin throughout the day and night. Instead of multiple daily injections, the pump delivers insulin continuously through a soft plastic tube called a line or giving set, which is connected to a small site on the skin. Under the skin sits a cannula—a tiny plastic or metal tube—that delivers the insulin. This site is changed every 2–3 days. Pumps use only fast-acting insulin (like Novorapid or Humalog), which allows for quicker and more flexible adjustments.
Basal insulin (background insulin)
Even when we’re not eating, our bodies still need small amounts of insulin to keep blood glucose levels steady. Without it, levels would slowly rise higher and higher. Instead of using a long-acting insulin once a day (like Lantus), the pump delivers tiny amounts of fast-acting insulin continuously, like a slowly dripping tap. This steady, low-level insulin is called basal insulin. The pump can adjust the drip rate at different times of the day and night to match what your child’s body needs—for example, more insulin overnight or less during periods of activity.
Bolus Insulin (For Food and Corrections)
In addition to basal insulin, the pump can give extra doses of insulin—called bolus insulin—when your child eats or has a high blood glucose level. To do this, you tell the pump:
Your child’s current blood glucose level (from a finger prick or sensor), and
How many carbohydrates they are about to eat.
The pump then calculates how much insulin is needed to cover the food and, if necessary, give a correction dose to bring down a high reading. This makes it easier to manage glucose levels around meals and helps avoid spikes or dips.
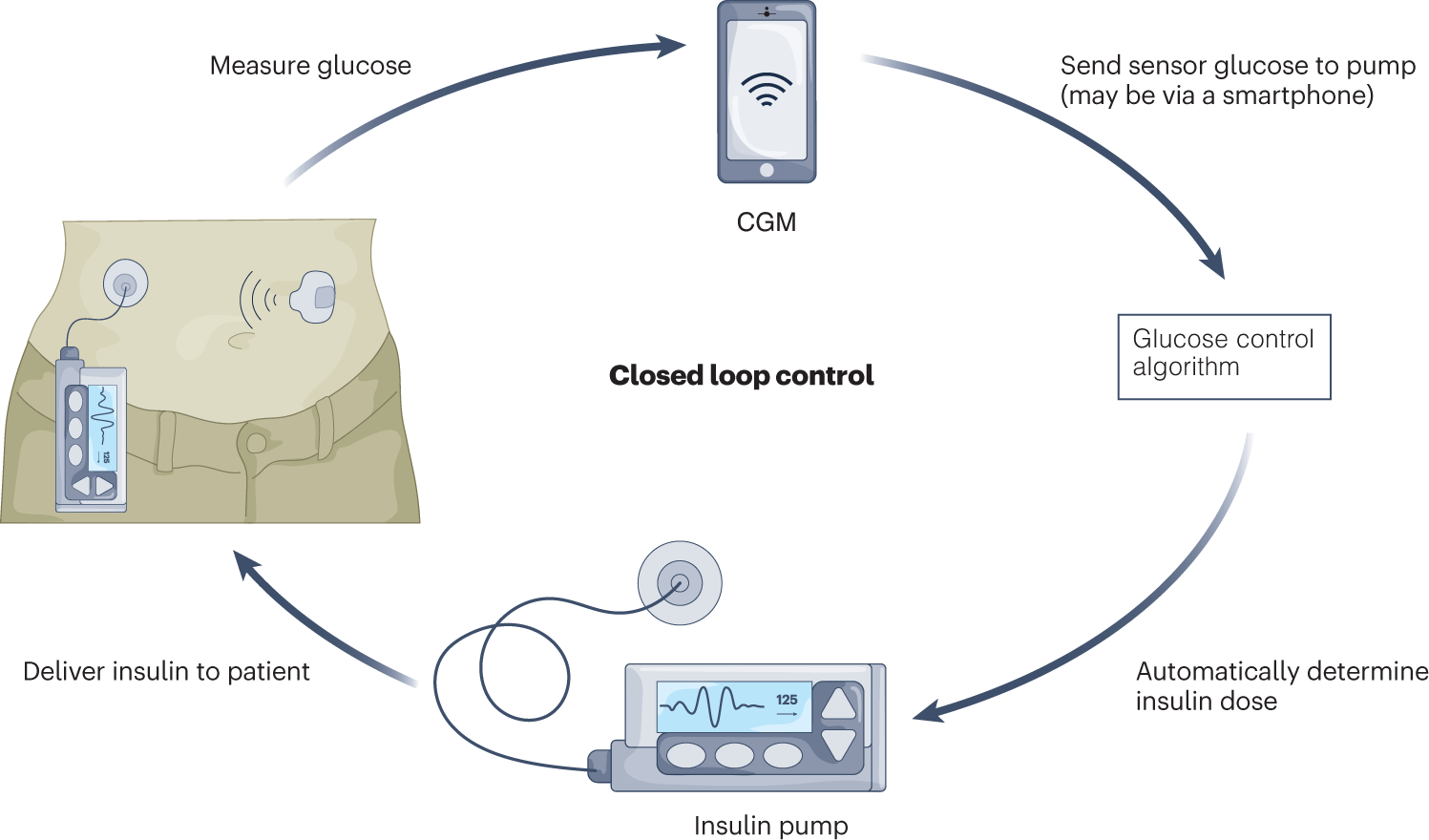
Hybrid Closed-Loop (HCL) Pumps
Some of the newer pumps use Automatic Insulin Delivery (AID), otherwise known as hybrid closed-loop systems (HCL). These work with a CGM (continuous glucose monitor) that automatically sends glucose readings to the pump. The pump uses this information to adjust insulin automatically, giving more insulin if glucose is rising or less insulin (or even pausing) if a low is expected.
If your child’s glucose is predicted to go high, the pump can increase the basal insulin or give a small automatic correction. If a low is predicted, it can reduce or stop insulin temporarily to help keep your child safe.
While AID pumps are smart and helpful, they still need you to enter the amount of carbohydrates your child is eating. This helps the pump work most effectively and prevents it from constantly trying to "catch up" with high levels after meals.
Using an insulin pump—especially with an automated insulin delivery system—can make managing diabetes easier and more flexible for tamariki and their whānau. Your diabetes team will support you to learn and use this technology . Ask your diabetes nurse or doctor if you would like to learn more about insulin pumps
Pumps give more accurate insulin delivery and allow different amounts to be eaten at different times. Pumps can also make it easier to adjust insulin doses for intensive sports regimes or during periods of sickness.
In New Zealand Pharmac fund insulin pumps and CGMs are funded for tamariki with Type 1 diabetes. Talk to your diabetes nurse or doctor at your diabetes clinic if you would like to know more about insulin pumping.
See also:
Think you've got it sorted? Let's go over the main points. Ready?
Think you've got it sorted now?
If you and your parent/carer have read through the information above and watched the videos, and you feel confident that you understand this topic, print off and fill in the evaluation form below (you might need to ask someone to print this off for you) and return to the nurse on your ward. If you have any questions, note them down on this form and your diabetes nurse specialist will discuss them with you.
Insulin Types and Regimens: Evaluation
My child and I have read the information above and watched the videos on insulin types and regimens. I understand the different insulin types and the insulin regimen my child is on.
| Yes | No | |
| Do you know the names of the insulin that your child will be using when you leave hospital? | ||
| Do you know how each of these insulins work? | ||
| Do you understand what an insulin pump is and how it works? | ||
| Do you know where to find more information if you are interested in starting an insulin pump? |
Comments:
Date:
Name:
